Guillain-Barré syndrome (GBS) post vaccination
Rare adverse event temporally associated with vaccination
Guillain-Barré syndrome (GBS) is a rapid-onset muscle weakness caused by the immune system damaging the peripheral nervous system. GBS post vaccination can occur with causality difficult to assess with occurrence frequency close to background frequency.
Hypothesis: Vaccinations can cause GBS onset in some vaccinees (rare frequency).
Literature evidence: GBS has been associated with influenza[1] and COVID-19 vaccinations[2]. GBS has been reported following Moderna[3–7], Pfizer BioNTech BNT162b2[8–16], Oxford AstraZeneca ChAdOx1 day[12,17–31], Johnson & Johnson/Janssen Ad26.CoV2.S[7,32–36], Sinopharm[30,31], and Sputnik V[31,37] COVID-19 vaccines. It has been suggested that many GBS patients are expected as sporadic cases and should not be considered causal[38]. For Pfizer BioNTech BNT162b2 mRNA vaccine, no increased incidence of GBS in a cohort of 3.9 million recipients was detected[39]. A review of GBS incidence in Vaccine Safety Datalink found an increased incidence following Ad.26.COV.2 but not BNT172b2 or mRNA-1273 vaccines[40]. An excess of GBS cases following AstraZeneca-Oxford ChAdOx1-S vaccination has also been identified[41]. An increased risk for GBS after first dose but not second dose of ChAdOx1 nCov-19 vaccination has been reported[42]. Warnings that rare GBS cases may link to Johnson & Johnson/Janssen and AstraZeneca vaccines have been issued[43]. One etiology model for GBS following COVID-19 vaccination is autoimmune autoantibodies[2]; but, no serum anti-ganglioside antibodies were found in 15 of 17 patients tested[44]. Nearly all GBS patients after COVID-19 vaccinations also had facial weakness or paralysis[40].
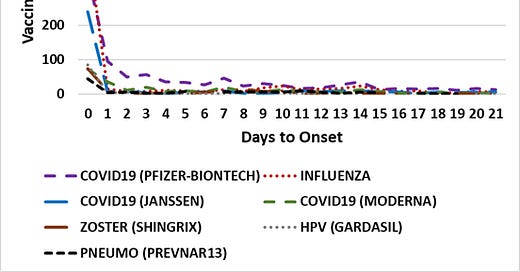
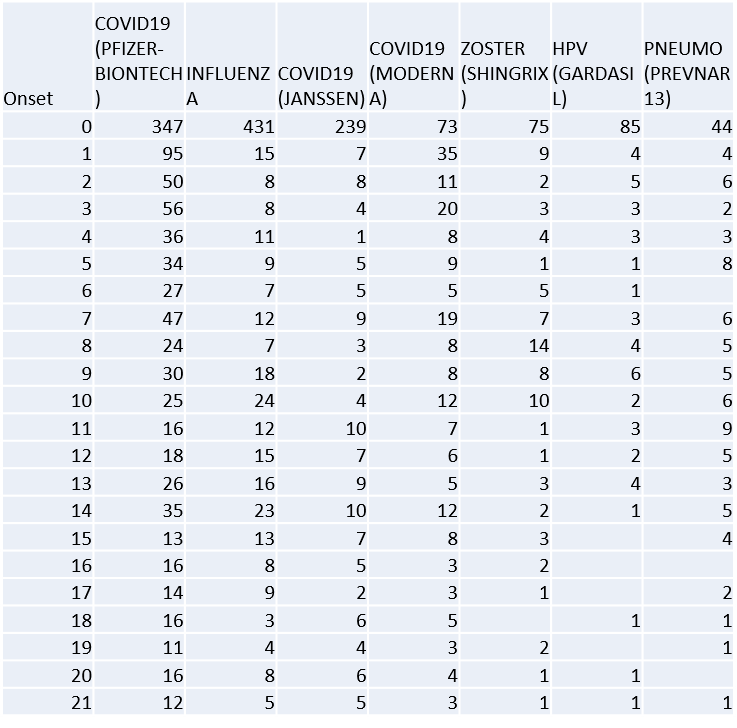
Vaccine Adverse Event Reporting System (VAERS) evidence: VAERS was data mined for reports of GBS post vaccination. The day of onset for seven vaccines are illustrated in Figure 1. The VAERS data indicate a non-random pattern with the highest number of reports within 24 hours of vaccination for multiple vaccines. Reporting bias is unlikely to account for this non-random pattern.
Figure 1. Guillain-Barré syndrome days to onset in VAERS[45]. Vaccines plotted include COVID-19 (Pfizer-BioNTech, Moderna, and Janssen), Influenza, Shingles Zoster (SHINGRIX), Human papillomavirus HPV (GARDASIL), and Pneumococcal PNEUMO (PREVNAR13).
This onset pattern is too rapid for molecular mimicry, epitope sharing, and autoimmune antibodies to be causative prior to day 7. Similar patterns shared by COVID-19, Influenza, Shingles Zoster, human papillomavirus, and Pneumococcal vaccines support innate immune responses as a major component of disease early etiology. Clinically, most GBS patients following COVID-19 vaccination showed typical demyelination neuropathy with albumin-cytological dissociation[46]; the timing suggests that demyelination neuropathy and albumin-cytological dissociation might be subsequent events in the disease etiology for patients with immediate onset adverse events. The immediate onset pattern of GBS following vaccination is different from the observed pattern for Zoster vaccines[47]; their reported Zoster vaccine onset pattern is consistent with the development of autoimmune antibodies in contrast to the immediate onset Zoster vaccine records in VAERS (Figure 1). Note that autoantibodies are detected for some GBS patients post COVID-19 vaccination[11,48]; onset of GBS for multiple patients is consistent with the development of autoantibodies[6,10–12,16,19–28]. Of these nine patients, four tested positive with with ganglioside antibody panel (2: anti-GM1, antig-GD1a, and anti-sulfatide)[37].
Innate Immune Responses & Peripheral Nervous System:
Consistent with the observed immediate onset of reported pain associated adverse events, innate immune response molecules are known to be associated with pain. These innate immune responses include the release of inflammatory molecules, including histamine, interleukin 1β (IL-1β), interleukin 6 (IL-6), monocyte chemoattractant protein (MCP-1), prostaglandin E2 (PGE2), tumor necrosis factor (TNF; formerly TNFα), etc.; these innate immune cells include macrophages, granulocytes including mast cells, T helper cells, and other immune cells[49–52]. PGE2 is a well-known lipid mediator that contributes to inflammatory, neuropathic, and visceral pain, see[52]. IL-1β, IL-6, and TNF are involved in the process of pathological pain[49]. Histamine is known to be algesic (cause pain) to peripheral nervous system[53].
Proposed GBS post vaccination etiology (ordered events):
• Vaccination: 1+ vaccines
• Innate immune system responds to vaccine
• Innate immune cells responses trigger GBS in some vaccinees with a low frequency
• Immune cells infiltration at blood-never barrier during inflammation (albumin-cytological dissociation)
• Some individuals with GBS develop autoantibodies post immune cells infiltration of peripheral nervous system
References
[1] Galeotti F, Massari M, D’Alessandro R, Beghi E, Chiò A, Logroscino G, et al. Risk of Guillain-Barré syndrome after 2010-2011 influenza vaccination. Eur J Epidemiol 2013;28:433–44. https://doi.org/10.1007/s10654-013-9797-8.
[2] Khan Z, Ahmad U, Ualiyeva D, Amissah OB, Khan A, Noor Z, et al. Guillain-Barre syndrome: An autoimmune disorder post-COVID-19 vaccination? Clin Immunol Communications 2022;2:1–5. https://doi.org/10.1016/j.clicom.2021.12.002.
[3] Dalwadi V, Hancock D, Ballout AA, Geraci A. Axonal-Variant Guillian-Barre Syndrome Temporally Associated With mRNA-Based Moderna SARS-CoV-2 Vaccine. Cureus 2021;13:e18291. https://doi.org/10.7759/cureus.18291.
[4] Bijoy George T, Kainat A, Pachika PS, Arnold J. Rare occurrence of Guillain-Barré syndrome after Moderna vaccine. BMJ Case Rep 2022;15:e249749. https://doi.org/10.1136/bcr-2022-249749.
[5] Matarneh AS, Al-battah AH, Farooqui K, Ghamoodi M, Alhatou M. COVID-19 vaccine causing Guillain-Barre syndrome, a rare potential side effect. Clin Case Rep 2021;9:e04756. https://doi.org/10.1002/ccr3.4756.
[6] Masuccio FG, Comi C, Solaro C. Guillain–Barrè syndrome following COVID-19 vaccine mRNA-1273: a case report. Acta Neurologica Belgica 2021. https://doi.org/10.1007/s13760-021-01838-4.
[7] Sriwastava S, Shrestha AK, Khalid SH, Colantonio MA, Nwafor D, Srivastava S. Spectrum of Neuroimaging Findings in Post-COVID-19 Vaccination: A Case Series and Review of Literature. Neurol Int 2021;13. https://doi.org/10.3390/neurolint13040061.
[8] Hughes DL, Brunn JA, Jacobs J, Todd PK, Askari FK, Fontana RJ. Guillain-Barré Syndrome After COVID-19 mRNA Vaccination in a Liver Transplantation Recipient With Favorable Treatment Response. Liver Transpl 2022;28:134–7. https://doi.org/10.1002/lt.26279.
[9] Aomar-Millán IF, Martínez de Victoria-Carazo J, Peregrina-Rivas JA, Villegas-Rodríguez I. COVID-19, Guillain-Barré syndrome, and the vaccine. A dangerous combination. Rev Clín Esp (Engl Ed) 2021;221:555–7. https://doi.org/10.1016/j.rceng.2021.05.002.
[10] Bouattour N, Hdiji O, Sakka S, Fakhfakh E, Moalla K, Daoud S, et al. Guillain-Barré syndrome following the first dose of Pfizer-BioNTech COVID-19 vaccine: case report and review of reported cases. Neurol Sci 2022;43:755–61. https://doi.org/10.1007/s10072-021-05733-x.
[11] Fukushima T, Tomita M, Ikeda S, Hattori N. A case of sensory ataxic Guillain–Barré syndrome with immunoglobulin G anti-GM1 antibodies following the first dose of mRNA COVID-19 vaccine BNT162b2 (Pfizer). QJM 2022;115:25–7. https://doi.org/10.1093/qjmed/hcab296.
[12] Kim JW, Kim YG, Park YC, Choi S, Lee S, Min HJ, et al. Guillain-Barre Syndrome After Two COVID-19 Vaccinations: Two Case Reports With Follow-up Electrodiagnostic Study. J Korean Med Sci 2022;37. https://doi.org/10.3346/jkms.2022.37.e58.
[13] Kim Y, Zhu Z, Kochar P, Gavigan P, Kaur D, Kumar A. A Pediatric Case of Sensory Predominant Guillain-Barré Syndrome Following COVID-19 Vaccination. Child Neurol Open 2022;9:2329048X221074549. https://doi.org/10.1177/2329048X221074549.
[14] Yamada S, Yamada K, Nishida H. A Case of Sequential Development of Polymyalgia Rheumatica and Guillain-Barré Syndrome Following Administration of the Pfizer-BioNTech COVID-19 Vaccine. Intern Med 2022;advpub. https://doi.org/10.2169/internalmedicine.0319-22.
[15] Trimboli M, Zoleo P, Arabia G, Gambardella A. Guillain-Barré syndrome following BNT162b2 COVID-19 vaccine. Neurol Sci 2021;42:4401–2. https://doi.org/10.1007/s10072-021-05523-5.
[16] Malamud E, Otallah SI, Caress JB, Lapid DJ. Guillain-Barré Syndrome After COVID-19 Vaccination in an Adolescent. Pediatr Neurol 2022;126:9–10. https://doi.org/10.1016/j.pediatrneurol.2021.10.003.
[17] Ogbebor O, Seth H, Min Z, Bhanot N. Guillain-Barré syndrome following the first dose of SARS-CoV-2 vaccine: A temporal occurrence, not a causal association. IDCases 2021;24:e01143. https://doi.org/10.1016/j.idcr.2021.e01143.
[18] Min YG, Ju W, Ha Y-E, Ban J-J, Lee SA, Sung J-J, et al. Sensory Guillain-Barre syndrome following the ChAdOx1 nCov-19 vaccine: Report of two cases and review of literature. J Neuroimmunol 2021;359. https://doi.org/10.1016/j.jneuroim.2021.577691.
[19] Biswas A, Pandey SK, Kumar D, Vardhan H. Post Coronavirus Disease‑2019 Vaccination Guillain‑Barré Syndrome. Indian J Public Health 2021;65:422–4. https://doi.org/10.4103/ijph.ijph_1716_21.
[20] Aldeeb M, Okar L, Mahmud SS, Adeli GA. Could Guillain–Barré syndrome be triggered by COVID-19 vaccination? Clin Case Rep 2022;10:e05237. https://doi.org/10.1002/ccr3.5237.
[21] Kanabar G, Wilkinson P. Guillain‐Barré syndrome presenting with facial diplegia following COVID‐19 vaccination in two patients. BMJ Case Rep 2021;14:e244527. https://doi.org/10.1136/bcr-2021-244527.
[22] Introna A, Caputo F, Santoro C, Guerra T, Ucci M, Mezzapesa DM, et al. Guillain-Barré syndrome after AstraZeneca COVID-19-vaccination: A causal or casual association? Clin Neurol Neurosurg 2021;208:106887. https://doi.org/10.1016/j.clineuro.2021.106887.
[23] McKean N, Chircop C. Guillain-Barré syndrome after COVID-19 vaccination. BMJ Case Rep 2021;14:e244125. https://doi.org/10.1136/bcr-2021-244125.
[24] Kripalani Y, Lakkappan V, Parulekar L, Shaikh A, Singh R, Vyas P. A Rare Case of Guillain-Barré Syndrome following COVID-19 Vaccination. EJCRIM 2021;8. https://doi.org/10.12890/2021_002797.
[25] Hasan T, Khan M, Khan F, Hamza G. Case of Guillain-Barré syndrome following COVID-19 vaccine. BMJ Case Rep 2021;14:e243629. https://doi.org/10.1136/bcr-2021-243629.
[26] James J, Jose J, Gafoor VA, Smita B, Balaram N. Guillain-Barré syndrome following ChAdOx1 nCoV-19 COVID-19 vaccination: A case series. Neurol Clin Neurosci 2021;9:402–5. https://doi.org/10.1111/ncn3.12537.
[27] da Silva GF, da Silva CF, Oliveira REN da N, Romancini F, Mendes RM, Locks A, et al. Guillain–Barré syndrome after coronavirus disease 2019 vaccine: A temporal association. Clin Exp Neuroimmunol 2022;13:92–4. https://doi.org/10.1111/cen3.12678.
[28] Patel SU, Khurram R, Lakhani A, Quirk B. Guillain-Barre syndrome following the first dose of the chimpanzee adenovirus-vectored COVID-19 vaccine, ChAdOx1. BMJ Case Rep 2021;14:e242956. https://doi.org/10.1136/bcr-2021-242956.
[29] Allen CM, Ramsamy S, Tarr AW, Tighe PJ, Irving WL, Tanasescu R, et al. Guillain–Barré Syndrome Variant Occurring after SARS-CoV-2 Vaccination. Ann Neurol 2021;90:315–8. https://doi.org/10.1002/ana.26144.
[30] Tabatabaee S, Rezania F, Alwedaie SMJ, Malekdar E, Badi Z, Tabatabaei SM, et al. Post COVID-19 vaccination Guillain-Barre syndrome: three cases. Hum Vaccin Immunother 2022;18:2045153. https://doi.org/10.1080/21645515.2022.2045153.
[31] Karimi N, Boostani R, Fatehi F, Panahi A, Okhovat AA, Ziaadini B, et al. Guillain-Barre Syndrome and COVID-19 Vaccine: A Report of Nine Patients. BCN 2021;12:703–10. https://doi.org/10.32598/bcn.2021.3565.1.
[32] Thant HL, Morgan R, Paese MM, Persaud T, Diaz J, Hurtado L. Guillain-Barré Syndrome After Ad26.COV2.S Vaccination. Am J Case Rep 2022;23:e935275-1-e935275-5. https://doi.org/10.12659/AJCR.935275.
[33] Zubair AS, Bae JY, Desai K. Facial Diplegia Variant of Guillain-Barré Syndrome in Pregnancy Following COVID-19 Vaccination: A Case Report. Cureus 2022;14:e22341. https://doi.org/10.7759/cureus.22341.
[34] Rossetti A, Gheihman G, O’Hare M, Kosowsky JM. Guillain-Barré Syndrome Presenting as Facial Diplegia after COVID-19 Vaccination: A Case Report. J Emerg Med 2021;61:e141–5. https://doi.org/10.1016/j.jemermed.2021.07.062.
[35] Prasad A, Hurlburt G, Podury S, Tandon M, Kingree S, Sriwastava S. A Novel Case of Bifacial Diplegia Variant of Guillain-Barré Syndrome Following Janssen COVID-19 Vaccination. Neurol Int 2021;13. https://doi.org/10.3390/neurolint13030040.
[36] Stefanou MI, Karachaliou E, Chondrogianni M, Moschovos C, Bakola E, Foska A, et al. Guillain-Barré syndrome and fulminant encephalomyelitis following Ad26.COV2.S vaccination: double jeopardy. Neurol Res Pract 2022;4:6. https://doi.org/10.1186/s42466-022-00172-1.
[37] Castiglione JI, Crespo JM, Lecchini L, Silveira FO, Luis MB, Cotti N, et al. Bilateral facial palsy with paresthesias, variant of Guillain-Barré syndrome following COVID-19 vaccine: A case series of 9 patients. Neuromuscul Disord 2022;32:572–4. https://doi.org/10.1016/j.nmd.2022.05.003.
[38] Lunn MP, Cornblath DR, Jacobs BC, Querol L, van Doorn PA, Hughes RA, et al. COVID-19 vaccine and Guillain-Barré syndrome: let’s not leap to associations. Brain 2021;144:357–60. https://doi.org/10.1093/brain/awaa444.
[39] García-Grimshaw M, Michel-Chávez A, Vera-Zertuche JM, Galnares-Olalde JA, Hernández-Vanegas LE, Figueroa-Cucurachi M, et al. Guillain-Barré syndrome is infrequent among recipients of the BNT162b2 mRNA COVID-19 vaccine. Clin Immunol 2021;230:108818. https://doi.org/10.1016/j.clim.2021.108818.
[40] Hanson KE, Goddard K, Lewis N, Fireman B, Myers TR, Bakshi N, et al. Incidence of Guillain-Barré Syndrome After COVID-19 Vaccination in the Vaccine Safety Datalink. JAMA Netw Open 2022;5:e228879–e228879. https://doi.org/10.1001/jamanetworkopen.2022.8879.
[41] Osowicki J, Morgan H, Harris A, Crawford NW, Buttery JP, Kiers L. Guillain-Barré Syndrome in an Australian State Using Both mRNA and Adenovirus-Vector SARS-CoV-2 Vaccines. Ann Neurol 2021;90:856–8. https://doi.org/10.1002/ana.26218.
[42] Keh RYS, Scanlon S, Datta-Nemdharry P, Donegan K, Cavanagh S, Foster M, et al. COVID-19 vaccination and Guillain-Barré syndrome: analyses using the National Immunoglobulin Database. Brain 2022:awac067. https://doi.org/10.1093/brain/awac067.
[43] Dyer O. Covid-19: Regulators warn that rare Guillain-Barré cases may link to J&J and AstraZeneca vaccines. BMJ 2021;374:n1786. https://doi.org/10.1136/bmj.n1786.
[44] Caress JB, Castoro RJ, Simmons Z, Scelsa SN, Lewis RA, Ahlawat A, et al. COVID-19-associated Guillain-Barré syndrome: The early pandemic experience. Muscle Nerve 2020;62:485–91. https://doi.org/10.1002/mus.27024.
[45] VAERS. Vaccine Adverse Event Reporting System. U.S. Department of Health & Human Services; 2021.
[46] Fernandez PEL, Pereira JM, Risso IF, Rodrigues Silva PB, Freitas Barboza ICF, Silveira CGV, et al. Guillain-Barre syndrome following COVID-19 vaccines: A scoping review. Acta Neurol Scand 2022;145:393–8. https://doi.org/10.1111/ane.13575.
[47] Goud R, Lufkin B, Duffy J, Whitaker B, Wong H-L, Liao J, et al. Risk of Guillain-Barré Syndrome Following Recombinant Zoster Vaccine in Medicare Beneficiaries. JAMA Intern Medi 2021;181:1623–30. https://doi.org/10.1001/jamainternmed.2021.6227.
[48] Scendoni R, Petrelli C, Scaloni G, Logullo FO. Electromyoneurography and laboratory findings in a case of Guillain-Barré syndrome after second dose of Pfizer COVID-19 vaccine. Hum Vaccin Immunother 2021;17:4093–6. https://doi.org/10.1080/21645515.2021.1954826.
[49] Zhang J-M, An J. Cytokines, inflammation, and pain. Int Anesthesiol Clin 2007;45:27–37. https://doi.org/10.1097/AIA.0b013e318034194e.
[50] Clark AK, Old EA, Malcangio M. Neuropathic pain and cytokines: current perspectives. J Pain Res 2013;6:803–14. https://doi.org/10.2147/JPR.S53660.
[51] Ricciotti E, FitzGerald GA. Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol 2011;31:986–1000. https://doi.org/10.1161/ATVBAHA.110.207449.
[52] Kawabata A. Prostaglandin E2 and Pain—An Update. Biol Pharm Bull 2011;34:1170–3. https://doi.org/10.1248/bpb.34.1170.
[53] Yu J, Lou G-D, Yue J-X, Tang Y-Y, Hou W-W, Shou W-T, et al. Effects of histamine on spontaneous neuropathic pain induced by peripheral axotomy. Neurosci Bull 2013;29:261–9. https://doi.org/10.1007/s12264-013-1316-0.